By Jeffrey Havenner
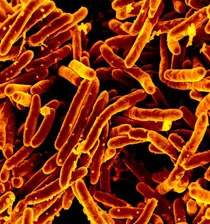
I watched the sun come up on December 22, 2012 with a certain satisfaction. It was the day after the predicted "end of the world" due to the expiration of the Mayan calendar. Little did I know, until I read it in an article on hospital-acquired infections, that we may be facing at the very least the end of another era of the usefulness of antibiotics in medicine. Has bacterial resistance really come to that? Some medical experts are suggesting so.
A favorite saying of Pasteur was that "chance favors the prepared mind." In the 1920s English physician Alexander Fleming was looking at some cultures of Staphylococcus aureus that were contaminated with the same blue green mold that is common on old bread. He could have destroyed the cultures and started over but instead he examined them and noticed that something about the mold seemed to be restricting the growth of the bacteria. Fleming is credited with discovering Penicillin, the first antibiotic.
Since that discovery, antibiotics have become a staple of medicine, as they are actual curative drugs. That is, antibiotics do not prevent one from getting a disease, as do vaccines. Instead they clear from the patient's system the actual causative agent of a disease after infection. Unfortunately, just as Sir Isaac Newton described the law of action and opposite reaction in physics the opposite reaction to antibiotics was antibiotic resistance in bacteria.
As time has gone on, microbiologists have described antibiotic resistance genes on plasmids and so called "pathogenicity islands" that can be transferred horizontally between bacteria occupying the same environments. Some pathogens have achieved multiple antibiotic resistance to the point that there are few treatment options left. Potential allergic reactions and toxic side effects complicate the picture even more.
The problem of antibiotic resistance is twofold. The most resistant forms of pathogens can lurk in hospital environments ready to infect patients with already compromised immune systems. Along with that the rate that new antibiotics are coming into clinical use has been declining steadily since the 1980s.
Commercially, antibiotics seem to be following the law of diminishing return. As bacteria become more proficient in acquiring resistance, a certain pessimism settles in that new antibiotics could even recoup the cost of R&D and the lengthy approval process by the FDA.
So what will happen? In one scenario the Government could take over antibiotic development and production largely by contracting with commercial entities similar to defense contracting. Antibiotic research and development could become the province of Non-Governmental Organizations. Ralph Winter envisioned groups of scientifically oriented Christians fighting disease in the name of God and not for personal fame or profit. Finally, new classes of drugs could be developed that target bacterial virulence mechanisms without necessarily killing them. These might become forms of maintenance and disease-management drugs that are more profitable in the long run. We will examine these in greater detail later.
Endnote:
This is the article referred to above: http://www.bethesdamagazine.com/Bethesda-Magazine/January-February-2013/The-KPC-Killer/. The incident caused quite a stir in the Washington DC area because it was a local event that occurred at the NIH in 2012.
Jeffrey Havenner is a retired microbiologist who serves the RWI as a scientific consultant.